by Ellie Bowen | Dec 7, 2023
Our first week of medical school at the University of Michigan this past summer, I sat in South Lecture Hall with 163 of my new classmates listening to incredible physicians share their philosophies on the practice of medicine. These lectures were inspiring, ranging from how to make the most out of your medical education to how to make the most out of not just your medical career, but your life. One lecture in particular struck me: Chris Sonnenday, MD, a transplant surgeon, talking to us about the small acts of care that make the biggest difference to patients.

I entered medical school recovering from a distal radial ulnar joint injury— not an ideal way to start, but UMMS worked with me to make accommodations and my counselor even helped me find an appointment with a hand surgeon in Ann Arbor!
Dr. Sonnenday is the Surgical Director of Liver Transplantation for Michigan Medicine, and he performs complex hepatobiliary, oncologic and liver transplantation surgery, while also leading numerous research studies. For someone with such intense responsibilities, he is remarkably down to earth. He coaches his kid’s soccer team and runs marathons in his free time. When he started talking about patient care, he emphasized that he just tries to give his patients the honesty and humanity that he would want from his doctor. He described how before each of the surgeries he does, he has made it a practice to hold the hand of his patient while they fall asleep under anesthesia. Oftentimes this is the only thing patients remember when they awake from surgery — that they weren’t alone.
I sat in the lecture hall moved practically to tears and tried to write down takeaways from the lecture I had just heard. This proved difficult, as I was still recovering from donning a cast all summer after dislocating my wrist, and so these notes were even more illegible than my usual bad handwriting. Luckily, I was able to clearly write down Dr. Sonnenday’s email, and I decided to reach out to him that day to let him know how impactful his talk had been to me. To my surprise he responded right away and offered to meet with me to talk about my interests.
Pursuing Professional Interests: AI, Transplant Research and Inspiring Role Models
When we met on Zoom, I shared that I was interested in artificial intelligence for medical use cases — the research I pursued before medical school — and he immediately connected me to the Transplant Research, Education, and Engagement (TREE) team, where I’ve since started on a research project using computational tools to help optimize organ donor-recipient matching. The TREE team is a multidisciplinary group of data scientists, researchers and surgeons who collaborate on research projects in smaller groups and share their learnings with one another and the scientific community through manuscript publishing. TREE meets weekly to go through project updates from the broader transplant group at Michigan Medicine, and my smaller research group working on the donor-matching algorithm meets biweekly.
In addition to research opportunities, faculty like Dr. Sonnenday are very willing to allow students to shadow them and learn from their clinical practice. I was lucky to get to spend a day shadowing Dr. Sonnenday in his Liver Tumor Clinic. I accompanied him to see his clinic patients, all of whom he had formed longitudinal relationships with and spent the full appointment time (and sometimes more) ensuring that he answered all their questions. After each patient visit, he took further time to thoroughly explain the disease etiologies and relevant lab findings to me in detail.
I learned a lot that day, not just about cancer pathology and anatomy, but about what it really looks like to be a good doctor: someone who is unhurried and generous with their time, always making sure to thoroughly teach patients about their conditions, as well as teach trainees about how to care for these patients. Seeing his kindness, honesty and genuine care for each of his patients — whether they were the first patient of the day or the last one at the end of a long day of clinic — was so inspiring and modeled the type of physician I want to be one day. Many of my friends in medical school have had similarly impactful shadowing experiences with Michigan physicians who love teaching med students, starting as early as M1 year.
Introduction to Interprofessional Collaborative Skills: Shadowing a Sex Therapist
Doctors aren’t the only professionals we learn from and shadow as students. An integral part of our first-year curriculum includes the interprofessional collaborative skills introduction (ICS-I), which includes shadowing various health professionals such as nurse practitioners, physical therapists, social workers, doulas, music therapists, dietitians, pharmacists and pathologists. My ICS-I assignments proved to be equally valuable learning experiences as my day shadowing at the Liver Cancer Clinic. I was assigned to shadow a music/pet therapist, a child audiologist and a sex therapist, a social worker who specializes in sexual health counseling.
My first day of shadowing was with Amy Raad, LMSW, CST, a sex therapist at the Center for Vulvar Diseases, and I had no idea what to expect. Little did I know this would turn out to be one of the most interesting days of medical school so far. Amy is an expert in sexual health, women’s health, intimate relationship distress and trauma recovery. She works with patients to help overcome any concerns about sexual health or function after major changes like those brought about through radiation treatment for cancer. She sees an array of patients with varying conditions, from diverse backgrounds and age groups.
Amy made such a big impact on her patients with her openness, depth of knowledge and empathy. She was able to help patients feel comfortable talking about sexual health and function with seeming ease (although I’m sure that’s harder than she made it look!), and it was really inspiring to see her meet patients where they are and create a space where they felt safe to share difficulties rendered by their diagnoses. She was also just insanely cool. Before shadowing in the clinic, I didn’t know anything about this field, but after spending my day with Amy I was so thrilled to be part of a hospital system that offers these resources to patients. I left the clinic that day feeling assured that I had made the right choice in deciding to study medicine at Michigan.

Enjoying a sunset over Lake Michigan during a weekend trip to Grand Haven.
Life Outside Medical School: Ann Arbor, Student Orgs and Quiz-Free Weekends!
When I first began medical school, I was nervous about not being able to keep up with my life outside of school. As a nontraditional student, things like spending time with my family and friends, cultivating artistic outlets and pursuing research had grown paramount to my wellbeing in the years since I’ve graduated college, and I’ve gotten so used to having ample time for them. I was worried that M1 year wouldn’t allow me time for these diverse interests. Luckily, that worry was pretty unfounded — if anything, I feel encouraged to pursue these interests by everyone from the faculty and health professionals I shadow who share the important non-medicine-specific interests in their lives, to my doctoring coach who checks in on my self-care goals first thing every time we meet.

Taking a ceramics class at Ann Arbor Art Center!
Ann Arbor also provides ample opportunity to explore new interests. On a whim I applied for a financial
scholarship to take a ceramics class at the Ann Arbor Art Center, and now I’ve spent one night every week learning how to throw on the wheel and am working on a set of funky (read: lopsided) mugs as Christmas gifts for my roommates. Ceramics classes have been a really fun way to make friends outside of medical school, and they’re just one example of the myriad activities Ann Arbor has to offer for students.
While there’s basically a student group at Michigan Med for just about anything you might be interested in, if you don’t happen to find exactly the group you want, it’s really easy to create your own student group. In fact, this year, three friends and I started the AI in Medicine club to gather students interested in learning about AI developments in the medical field, host talks from faculty working in this field, connect students with research opportunities, and discuss ethical challenges of incorporating ever-advancing AI technology into our healthcare system.

Some med school friends during a camping trip to Sleeping Bear Dunes this fall (feat. Christopher the best dog ever).
Aside from these more organized activities, it’s been really fun just getting to know my amazing classmates. Since we have a non-quiz weekend approximately every two weekends, we take advantage of the free time to do things like go camping at Sleeping Bear Dunes, visit Lake Michigan, and host dinner parties. With all the rich opportunities for personal and professional growth afforded by Michigan Medicine, I’ve had an M1 year that has so far exceeded any and all expectations I had coming in. I can’t wait for what’s to come in my clinical year.
Ellie Bowen is a first-year student at the University of Michigan Medical School originally from Grand Rapids, Michigan. In her free time she enjoys spending time with her niece and nephew in Ann Arbor, practicing yoga, and getting out in nature with friends. She can be followed on X @ellierosebowen.
by Hannah Slater & Grace Tremonti | Nov 27, 2023
Coming into medical school, we knew we wanted to make an impact in the University of Michigan Medical School (UMMS) community by following our passion for improving equity, representation and inclusion. One student group that particularly caught our attention was the Student Diversity Council (SDC), which works to ensure the medical school community promotes diversity, equity, inclusion, accessibility and justice (DEIAJ). SDC also works closely with the administrators to amplify student voices in various medical school decisions.
 Following a small group discussion in the medical student lounge (also known as the Slounge), we discovered our mutual interest in diversity promotion. We reached out to the leadership team of SDC hoping to find a way to make an impact, specifically how we might be able to help improve our M1 curriculum. We were shocked and thrilled by how receptive SDC was to our ideas and passion for improving DEIAJ in the curriculum and how they welcomed us with open arms. Every member of SDC comes to the group with their own personal motivations and ideas for initiatives, so we felt we had a lot of support and resources to help us enact our own project!
Following a small group discussion in the medical student lounge (also known as the Slounge), we discovered our mutual interest in diversity promotion. We reached out to the leadership team of SDC hoping to find a way to make an impact, specifically how we might be able to help improve our M1 curriculum. We were shocked and thrilled by how receptive SDC was to our ideas and passion for improving DEIAJ in the curriculum and how they welcomed us with open arms. Every member of SDC comes to the group with their own personal motivations and ideas for initiatives, so we felt we had a lot of support and resources to help us enact our own project!
Our first project centered around patient presentations in the Scientific Trunk, the first year of pre-clinical studies at UMMS. Patient presentations are sessions where real patients tell their story and answer questions directly from students. While patient presentations during the Scientific Trunk served as opportunities to learn about the pathophysiology of disease, we found that students wanted to hear more about the impact of socioeconomic status, race and ethnicity on the patients’ health and journey through the health care system.
We worked alongside Hana Murphy, a fourth-year medical student, to conduct a survey to assess students’ thoughts about diversity in patient presentations. The overwhelming opinion from students was that they wanted to hear more from patients of diverse backgrounds, including representation of different race, ethnicity, gender, socioeconomic status, sexuality, educational status and ages. We brought the results of the survey and ideas for strategies to improve patient presentations to the Scientific Trunk faculty. We discovered the Office of Patient Experience, a department within Michigan Medicine that integrates patient perspectives by sharing their stories with the goal of maintaining and strengthening a patient-centered culture of care.
Our idea was to incorporate videos of patient stories from the Office of Patient Experience website into the Scientific Trunk. As a team, we went through each video and designated which part of the curriculum each story would best supplement. This helped contextualize the pathophysiology of specific disease processes with real-life patient experiences with more varied backgrounds. With the help of Scientific Trunk faculty, we were able to begin to more officially integrate these resources into the M1 curriculum.
As we progressed through our M1 year and the M2 clinical year rapidly approached, we began to think about how we could continue to incorporate values of DEIAJ into our education. Hana shared an experience she had prior to her emergency medicine clerkship where Dr. Marcia Perry, Assistant Professor and Associate Chair for Diversity, Equity and Inclusion in the Department of Emergency Medicine, and Dr. Samantha Chao, PGY-4 in Emergency Medicine, discussed strategies to minimize bias in clinical notation. She thought that the messages from their talk could be incredibly valuable to students before they entered the clinical setting, and we agreed.
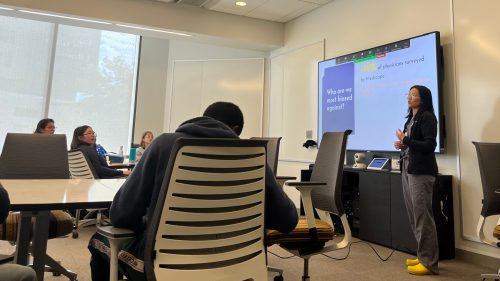
Dr. Chao presenting at the lunch event.
SDC hosted “The Power of Language in Clinical Documentation,” a lunch event to incoming M2s led by Drs. Perry and Chao. They led an interactive discussion about their experiences in the Emergency Department and their process of writing and presenting patient information while minimizing bias in their care teams. We looked at examples of notes with biased language and how it might influence providers’ perceptions of patients. They provided us with strategies to advocate for patients as medical students, acknowledging that we are in a position where we might not always feel empowered to correct a resident or attending. These strategies included changing progress notes to remove stigmatizing language and add person-centered phrasing. Other strategies included using the correct language during presentations on rounds, even when other providers might be using biased language.
In just two months of being clinical students, we are already able to put what we learned into practice. After inheriting a patient who had been through many medical services, his “one-liner,” the very first sentence anyone reads about them when looking through his medical chart, described the patient as a “drug abuser.” Changing the one-liner from “drug abuser” to “patient with a substance use disorder” was a small but tangible action toward reducing bias in the clinical space.
While clerkships take a lot of our time, our projects are still ongoing. As we traverse the clinical space, we are mindful of our current experiences and how they will inspire us to take action in the future. If you are reading this and are similarly passionate about DEIAJ work and want to have an impact, please consider working with or supporting the efforts of SDC!
Hannah Slater is a second-year medical student at the University of Michigan Medical School who is passionate about working with stigmatized and under-resourced communities. When not running around the hospital, you can find her baking bagels with friends, discovering new coffee shops with her partner or walking alongside the Huron River.
Grace Tremonti is a second-year medical student at the University of Michigan Medical School from Ann Arbor, MI. She is passionate about health policy, improving DEIAJ in the academic and clinical spaces and playing soccer!
by Kennedy S. Miller | Oct 26, 2023
After attending Second Look at Michigan (SL@M), it was clear that the University of Michigan Medical School was the place for me to pursue my medical education. However, the beginning of my medical school journey was bittersweet.
As it is for many matriculants, I had spent most of my life working towards becoming a physician, but I found myself not wanting to leave the life I had built for myself in DC. I was passionate about my work at the DC Primary Care Association (DCPCA) and had fallen in love with DC’s culture and pace of life. Collaborating with DC’s Federally Qualified Health Centers was immensely fulfilling, and I was sad to leave my projects, especially the initiatives that aimed to improve the holistic wellbeing of DC’s underserved patients.
Moreover, I had never lived in Michigan before, and I wasn’t sure where to start when it came to learning about the health infrastructure of my new community. I was intimidated by the prospect of starting over, both personally and professionally, in a new place. Crazily enough, it was a chance bus ride to West Ann Arbor that put my worries to rest and helped me get involved with the community health work that I hoped to continue upon moving to Michigan.
On June 16th, my best friend and I drove a U-Haul stuffed to the brim with everything I own from DC to Michigan. I moved here a couple months before starting school because I knew that I would need time to settle into my new life. For me, a huge part of feeling at home in a new place is exploring my community, so I made it a point to take public transit and visit different community gathering spaces around town. Some early-July day, while taking the bus to one of Ann Arbor’s district libraries, I happened to sit directly across from an advertisement for the Corner Health Clinic. It was a vibrant flier, with lots of playful icons and smiling faces. It stated that the clinic was a community health center that provided primary care to young folks in the Ypsilanti community. The flier also listed the clinic’s services, and two caught my attention: the community pantry and gender-affirming care.

A commemorative selfie to celebrate my first shadowing experience as a medical student.
Fortuitously, the clinic manifested in my life again a few weeks later, when Dr. Emad Abou-Arab, who happens to work at Corner Health Clinic one day a week, came to speak with the LEAD cohort about practicing medicine after the pandemic. During his talk, he spoke about his passion for community health. He described how difficult it is for physicians to operate within the strict, arbitrary confines that insurance imposes on the provision of health care. He shared with us some of the strategies he uses to work around these issues and improve his patients’ ability to access care. Dr. Abou-Arab exemplifies the kind of physician and advocate I hope to become, so I reached out to him and asked if I could shadow him at Corner Health. He agreed and said he was excited to have me join him in the clinic. I took the bus over to Ypsilanti and we spent the morning seeing patients.
Genevieve Mulligan, a fourth-year medical student applying into family medicine, was also at the clinic that day as part of her clinical rotations. At the beginning of the day, Dr. Abou-Arab invited Genevieve to “run the show.” I accompanied Genevieve to the patient room and observed her perform the interview. It was inspiring to see Genevieve ask insightful questions and invite the patients to speak on all aspects of their health. Genevieve has an incredible passion for family medicine and is a generous peer mentor and teacher, who fervently shared her knowledge with me. After concluding the patient interview, we then returned to the office, reported our findings to Dr. Abou-Arab, and developed a preliminary course of action, making sure to consider the patient’s unique circumstances. All three of us then entered the patient room to collaborate with them to finalize the treatment plan.
Though I have been interested in gender-affirming care for many years, this was my first real clinical experience with this branch of medicine. It was rewarding to see how relieved and excited the patients were to be receiving hormone replacement therapies. It was amazing to see that Ypsilanti community members could not only get their primary care needs addressed at the clinic, but also receive life-saving treatments that have historically been withheld (and, in some states, continue to be) from patients. It was also meaningful to think about the impact that receiving these treatments would make on the patients’ emotional wellbeing on a daily basis. Unfortunately, identities are frequently forced upon us. Holding identities that aren’t readily apparent to others can be painful because society places us in boxes that don’t always match the ones that we would choose for ourselves. For this reason, there is indescribable power in reclaiming one’s ability to define their own selves and impact how they are perceived by those around them. I am glad that places like the Corner Health Clinic exist because every time that a patient who is transitioning takes a dose of their medication, they are moving forward in their journey to embodying the person who they know themselves to be.

Volunteering at the Packard Health Fair, another community health opportunity I’ve gotten the chance to be a part of since becoming a medical student at UMMS.
After we finished seeing patients, Genevieve and I went to the bottom floor of the clinic, where the community pantry is housed. It offers healthy foods, baby clothes, toiletries, and basic household necessities for free to Ypsilanti’s youth. While working at DCPCA, I learned that medical care alone does not make a significant impact on a patient’s health if their basic needs, like housing, food, and safety, are not being met. Therefore, health care providers must consider these external determinants of health and provide wraparound care and integrated resources that work beyond patients’ medical needs to ensure their physical and emotional wellbeing. In-house services like the clinic’s community pantry help do exactly that.

The ad that I saw for the first time in July and again on my way home from shadowing Dr. Abou-Arab at the Corner Health Clinic.
At the end of the morning, I thanked Dr. Abou-Arab and Genevieve for their time and enthusiasm for helping me learn. I got on the bus back to Ann Arbor and upon taking my seat, I saw something colorful out of the corner of my eye. You wouldn’t believe me if I told you that I found myself sitting across from the very Corner Health Clinic flier that I had seen on my bus ride to the library in July.
The word that best encapsulates my time so far at UMMS is serendipity. Though it was hard to leave DC, a series of chance interactions have catapulted me into incredible opportunities that make me feel as though I am exactly where I am supposed to be, and I am grateful for that.
Kennedy S. Miller (she/hers) is a first-year medical student at the University of Michigan Medical School. Kennedy is passionate about community health, health equity, primary care,
and surgery.
by Aasma Hossain | Oct 5, 2023
 MedART is a longitudinal art therapy class for medical students at the University of Michigan that creates a space for discussion and creative expression. The program was founded in March 2022 by a group of friends looking to meaningfully reflect upon and convey their experiences in medical school. This is a course created by medical students for medical students. We found a need to provide a long-term creative outlet for processing the unique experiences that medical students encounter, and the novel emotions that our peers face with limited time and resources to share and understand them.
MedART is a longitudinal art therapy class for medical students at the University of Michigan that creates a space for discussion and creative expression. The program was founded in March 2022 by a group of friends looking to meaningfully reflect upon and convey their experiences in medical school. This is a course created by medical students for medical students. We found a need to provide a long-term creative outlet for processing the unique experiences that medical students encounter, and the novel emotions that our peers face with limited time and resources to share and understand them.
The course started off with the idea of making art more accessible to medical students as a means to relieve stress and promote well-being. The University of Michigan Medical School has several amazing events and workshops dedicated to promoting well-being through the arts. However, we felt there was a gap between having a space where students interested in the arts could really delve into it regularly, and providing an environment where they can feel safe to be vulnerable and have access to the creative medium. We decided to bridge this gap by introducing our peers to art therapy.
 The MedART Therapy course comprises eight sessions, led by our amazing art therapist, Dr. Katherine Munter, whose passion and dedication has been invaluable. The course focuses on topics such as grappling with perfectionism, body image, imposter syndrome, processing trauma, and reclaiming one’s identity as an individual through color theory, surrealism, tactile art, resourceful art, “anabolic” and “catabolic” art, and cultivating art from nature. Different from other art-based wellness programs that emphasize the visualization of art, MedART Therapy approaches healing and rejuvenation through the creation of art.
The MedART Therapy course comprises eight sessions, led by our amazing art therapist, Dr. Katherine Munter, whose passion and dedication has been invaluable. The course focuses on topics such as grappling with perfectionism, body image, imposter syndrome, processing trauma, and reclaiming one’s identity as an individual through color theory, surrealism, tactile art, resourceful art, “anabolic” and “catabolic” art, and cultivating art from nature. Different from other art-based wellness programs that emphasize the visualization of art, MedART Therapy approaches healing and rejuvenation through the creation of art.
 This notion of “process art” is core to our mission of empowering students, through art, to reframe personal struggles as opportunities for exploration, discovery and reflection. Students have found this course to provide an opportunity “to not be perfect, to be silly, to make friends, and to be mindful of what is going on around [them]”, and “learn to be more introspective… [using] different mediums to explore emotions and thought.”
This notion of “process art” is core to our mission of empowering students, through art, to reframe personal struggles as opportunities for exploration, discovery and reflection. Students have found this course to provide an opportunity “to not be perfect, to be silly, to make friends, and to be mindful of what is going on around [them]”, and “learn to be more introspective… [using] different mediums to explore emotions and thought.”
 Due to the success of the course last year, we have brought it back this fall and hope to establish it as a permanent elective available to medical students in the future. Today, MedART is a supportive community of learners spanning different cohort years, backgrounds, and interests who are all on this very outlandish journey we call medical school.
Due to the success of the course last year, we have brought it back this fall and hope to establish it as a permanent elective available to medical students in the future. Today, MedART is a supportive community of learners spanning different cohort years, backgrounds, and interests who are all on this very outlandish journey we call medical school.
Special thanks to Dr. Joel Howell, Dr. Thomas Sisson, the Department of Internal Medicine, the Learner’s Wellbeing Office, and everyone involved in creating and establishing this course.
Aasma Hossain is rising M3, currently on a leave of absence. Aasma lived in Bangladesh from the ages five to 10. She went on to graduate from Penn State in 2019 with a degree in biology and psychology, followed by two years of neurodegenerative disease and axonal technology research at the NIH. She has a background in the visual arts and loves reading, doing arts and crafts, and she is the proud parent of 100+ plants.
by Maya Hammoud | Sep 25, 2023
Wilderness Medicine is easily the most unique rotation I’ve done in medical school. Run by the Department of Emergency Medicine, Wilderness Medicine teaches students how to provide quality medical care in outdoor settings with limited resources, while also offering immersive experiences in backpacking, rock climbing, caving, and more! Join me as I take you through my past month on this interesting and exciting rotation.

Camping at Pictured Rocks.
In the first week, we jumped right in with outdoor activities and lectures, interactive patient cases that may arise in the wild, a mass casualty simulation event, and orienteering. We learn by listening, but also by doing. Class is fun, engaging, and interactive.
The next week, we backpacked through Pictured Rocks in northern Michigan. The week was filled with beautiful experiences in nature, long hikes, daily “fireside chats” where students educate the group on a topic of their choosing, swimming in Lake Superior, learning to obtain and filter water in the wild, and, of course, camping at a new site each day. By the end of the week, we had developed a strong sense of comradery and accomplishment having backpacked 43 miles together through hot weather at first, then cold and rainy weather, all while fighting off blisters and mosquitos. Despite the struggles at times, the beauty of the nature around us, the freedom of being “unplugged” from phones and social media, and the independence of traveling by foot with all of our food, shelter, and supplies contained in backpacks provided a spectacular and unforgettable experience.

Backpacking at Pictured Rocks.
We had less than a week before our next trip, but in that time we managed to squeeze in kayaking, attending regional wilderness medicine rounds, mountain biking, and daily lectures.
Our next trip, and frankly my favorite part of the course, included rock climbing in Kentucky and caving in Indiana. I, along with several of my classmates, had never done either of these activities before, but we soon learned that we were to be led by experts and could make remarkable progress with no prior experience necessary!

Climbing and belaying at the Red River Gorge.
We rock climbed in the Red River Gorge in Kentucky, a beautiful spot with thousands of natural rock walls of various heights and difficulty levels. It was great trying out the different climbs and watching our experienced resident leaders – Matt and Carlos – climb the more difficult rock walls. It was especially inspiring to see classmates who had a fear of heights overcome these fears and ascend multiple climbs! Climbing by day, we spent the evenings camping at Miguel’s and eating dinner at local spots in the small town of Slate, Kentucky.

Dinner at Miguel’s.
After two eventful days of climbing, we drove up to Buckner Cave in Indiana. Here, we learned about and experienced exploring a “wild cave,” led by expert cavers Anmar and Jess. At times, the cave was barely a foot and a half tall, necessitating belly crawling or rolling to move forward. In other spots, we climbed up or down narrow passages, navigated around obstacles, or, rarely, were able to walk through open spaces.
We learned tricks to avoiding hypothermia in caves (hint: it involves a contractor bag and a candle!), medical considerations for evacuating patients from caves, and basic geology on how and why caves form. We also had a moment where everyone turned off their headlamps and sat perfectly still so we could meditate in the pitch-black darkness and perfect silence that is unique to caves. We debriefed and celebrated this unique experience with smores and hot dogs around the campfire on our last night camping together as a group.
The following day, having explored the cave once, we did a simulated evacuation of a “patient” (one of our classmates) from the cave. It required extensive teamwork and coordination, but we managed to carry our classmate out on a “litter” (similar to a stretcher) through all of the obstacles and tight spaces of the cave to safety.

Extricating our “patient” from the cave.
After a team lunch, we drove back to Ann Arbor where we would finish up the course with a series of evidence-based medicine talks and a final exam of both written questions and scenario-based stations. Each student gave a talk on a wilderness medicine topic of their choosing, from managing obstetric emergencies in the wilderness to things that can go wrong while scuba diving or summiting mountains to the efficacy and importance of bug spray and sunscreen in the wild. We learned from each other, as we had throughout the course, both inside and outside of the classroom.

Sunset on Lake Superior.
As I reflect on the past month, I am in awe of how many new and unique experiences I have had in such a short span of time, as well as by the wealth of knowledge I have acquired on such a wide variety of wilderness medicine topics. Watching the sunset on Lake Superior, camping under the stars, scaling large rock walls in Kentucky, and exploring a cave 80 feet underground in Indiana were experiences my classmates and I will never forget. I wholeheartedly recommend this course for any student or prospective student whether or not they plan to pursue a career in wilderness medicine. I am so grateful for the amazing opportunity this course provided, as well as for the incredible resident and faculty leaders that made it happen.
Maya Hammoud is a fourth-year medical student at the University of Michigan. She is pursuing a career in general surgery, with an emphasis on medical education, clinical outcomes research, and improving diversity, equity, and inclusion in healthcare. In her free time she enjoys gymnastics, swimming, hiking, and reading.





 Following a small group discussion in the medical student lounge (also known as the
Following a small group discussion in the medical student lounge (also known as the 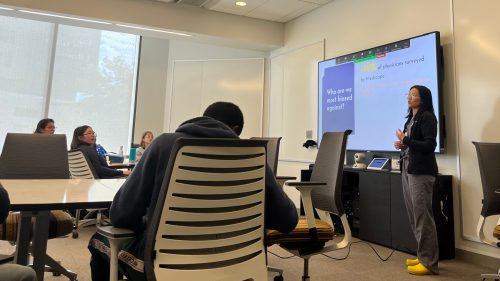



 MedART is a longitudinal art therapy class for medical students at the University of Michigan that creates a space for discussion and creative expression. The program was founded in March 2022 by a group of friends looking to meaningfully reflect upon and convey their experiences in medical school. This is a course created by medical students for medical students. We found a need to provide a long-term creative outlet for processing the unique experiences that medical students encounter, and the novel emotions that our peers face with limited time and resources to share and understand them.
MedART is a longitudinal art therapy class for medical students at the University of Michigan that creates a space for discussion and creative expression. The program was founded in March 2022 by a group of friends looking to meaningfully reflect upon and convey their experiences in medical school. This is a course created by medical students for medical students. We found a need to provide a long-term creative outlet for processing the unique experiences that medical students encounter, and the novel emotions that our peers face with limited time and resources to share and understand them. The MedART Therapy course comprises eight sessions, led by our amazing art therapist, Dr. Katherine Munter, whose passion and dedication has been invaluable. The course focuses on topics such as grappling with perfectionism, body image, imposter syndrome, processing trauma, and reclaiming one’s identity as an individual through color theory, surrealism, tactile art, resourceful art, “anabolic” and “catabolic” art, and cultivating art from nature. Different from other art-based wellness programs that emphasize the visualization of art, MedART Therapy approaches healing and rejuvenation through the creation of art.
The MedART Therapy course comprises eight sessions, led by our amazing art therapist, Dr. Katherine Munter, whose passion and dedication has been invaluable. The course focuses on topics such as grappling with perfectionism, body image, imposter syndrome, processing trauma, and reclaiming one’s identity as an individual through color theory, surrealism, tactile art, resourceful art, “anabolic” and “catabolic” art, and cultivating art from nature. Different from other art-based wellness programs that emphasize the visualization of art, MedART Therapy approaches healing and rejuvenation through the creation of art. This notion of “process art” is core to our mission of empowering students, through art, to reframe personal struggles as opportunities for exploration, discovery and reflection. Students have found this course to provide an opportunity “to not be perfect, to be silly, to make friends, and to be mindful of what is going on around [them]”, and “learn to be more introspective… [using] different mediums to explore emotions and thought.”
This notion of “process art” is core to our mission of empowering students, through art, to reframe personal struggles as opportunities for exploration, discovery and reflection. Students have found this course to provide an opportunity “to not be perfect, to be silly, to make friends, and to be mindful of what is going on around [them]”, and “learn to be more introspective… [using] different mediums to explore emotions and thought.” Due to the success of the course last year, we have brought it back this fall and hope to establish it as a permanent elective available to medical students in the future. Today, MedART is a supportive community of learners spanning different cohort years, backgrounds, and interests who are all on this very outlandish journey we call medical school.
Due to the success of the course last year, we have brought it back this fall and hope to establish it as a permanent elective available to medical students in the future. Today, MedART is a supportive community of learners spanning different cohort years, backgrounds, and interests who are all on this very outlandish journey we call medical school.




