by Alexandra Vita & CJ Schellack | Jul 21, 2023
Throughout medical school, we have the privilege of meeting patients with so many different life experiences. The physiology and pharmacology of medical illness is complex, but oftentimes we see that the external factors that lead to illness or injury are just as complex.
We’ve met patients with lung cancer, who have been exposed to heavy amounts of pollutants after factories were built close to their homes. We’ve seen people come into the emergency room with raging infections, who had to put off health care because they couldn’t afford the cost.
 It is an honor to be with patients in these moments and support them in ways that we can. However, sometimes it feels like there are constraints within the healthcare system — we leave these patient interactions wishing there was more we could do to change these peoples’ circumstances. This desire to drive positive change for patients beyond the one-on-one clinical setting often takes shape in the form of advocacy work.
It is an honor to be with patients in these moments and support them in ways that we can. However, sometimes it feels like there are constraints within the healthcare system — we leave these patient interactions wishing there was more we could do to change these peoples’ circumstances. This desire to drive positive change for patients beyond the one-on-one clinical setting often takes shape in the form of advocacy work.
Dr. Megan Purdy, a recent UMMS graduate, created a longitudinal course alongside U-M emergency medicine physician Dr. Brad Uren that allows students to develop skills in advocacy. In the first class, many students talked about experiences where they noticed barriers to care. People had interests about access to care for OB-GYN populations, immigrant and refugee populations, incarcerated populations, patients with substance use disorder, and more. Everyone expressed the hope to address inequities in healthcare, but felt they needed guidance about how to effectively start.
The class was a small group format, with regular guest speakers and opportunities for questions and answers with the guests after their prepared comments. Some of the pilot class’s favorite speakers are listed below.
The course kicked off with a meeting with Dr. Kermit Jones, an internal medicine physician whose experiences drove him to run for office in California’s 3rd Congressional District. He candidly shared what he learned from running a campaign, and he encouraged us to amplify the voices of our patients. He reminded us that “If you’re not at the table, you’re on the menu.”
We met former U.S. Surgeon General Dr. Jerome Adams, who spoke about his experiences in the White House and how to serve communities from a national lens. He chatted with each student individually, providing thoughts and guidance about our specific interests.
We met with Megan Groen, the senior advisor to the Director of the Michigan Department of Health & Human Services who spoke about the recent successes and the future goals of MDHHS. Students working at the U-M Student-Run Free Clinic were vocal about how insurance and food security were large concerns of patients, and Ms. Groen directed students to different resources and programs to address these issues.
Dr. Rahul Gupta, the Director of National Drug Control Policy, appointed by President Biden as the first physician to hold that role, led a discussion about the landscape of the opioid epidemic and the different policies and programs that have recently come into effect.
This class created a unique space where every week, students had the rare opportunity to have in-depth discussions with people who have worked in policy and advocacy for decades. In a welcoming and low-pressure environment, students were encouraged to bring up their hopes and concerns. In turn, experts gave students advice about how to pursue their ideas. We worked with the Michigan Medicine communications team to learn about effective ways to write an op-ed. From chatting with the manager of state and federal government relations from the Michigan State Medical Society, we learned how to advocate for our interests with our local representatives.
 At the end of the course, students had the opportunity to travel to Lansing, where they spoke with Washtenaw County’s Rep. Carrie Rheingans and Sen. Jeff Irwin. Some students interested in emergency medicine elected to travel to Washington, D.C. and attend the American College of Emergency Physician’s Leadership and Advocacy Course with Dr. Uren. In future classes, students may also travel to the American Medical Association’s National Advocacy Conference in Washington DC. Other opportunities may be available for students with other specialty interests as well.
At the end of the course, students had the opportunity to travel to Lansing, where they spoke with Washtenaw County’s Rep. Carrie Rheingans and Sen. Jeff Irwin. Some students interested in emergency medicine elected to travel to Washington, D.C. and attend the American College of Emergency Physician’s Leadership and Advocacy Course with Dr. Uren. In future classes, students may also travel to the American Medical Association’s National Advocacy Conference in Washington DC. Other opportunities may be available for students with other specialty interests as well.
This class provided networking opportunities, taught us tangible skills and instilled hope that we can leverage our perspective as medical students to advocate for our patients’ well-being. We are excited to continue this course and invite students to join this upcoming Fall and Winter!
by Blake Hardin | Jul 20, 2023
Currently more than 1 in 4 adults in the United States in the United States have some form of disability, as reported by the Centers for Disease Control and Prevention. While disability affects many individuals in the U.S. and worldwide, this population is one of the most unrecognized groups and faces significant health disparities.
Individuals with disabilities struggle with healthcare access, as 1 in 4 adults with disabilities ages 18-44 years do not have a usual healthcare provider. Additionally, 1 in 5 adults with disabilities have an unmet healthcare need because of cost in the past year, and 1 in 4 adults with disabilities 45 to 64 years did not have a routine check-up in the past year.
Furthermore, people with disabilities report feeling unsatisfied with the healthcare they receive significantly more than people without disabilities. This could be partially explained by the fact that more than eighty percent of physicians in the U.S. believe those with disabilities have a worse quality of life than those without disabilities, which may significantly impact the quality of care physicians provide to these patients. Disability can impact many facets of one’s life, so people with disabilities need comprehensive and empathetic care from physicians who have been trained to provide culturally competent healthcare.

MSDHA members at a BBQ social event during Summer 2022.
Growing up with a chronic illness, I have firsthand knowledge and experience of the stigmatization and isolation one can face by having a disability or chronic illness outside of the healthcare setting. While I was fortunate to have a great healthcare experience, I know from friends and loved ones that this is often not the case. I was heavily involved in a disability advocacy group during undergrad to bring these issues to light and amplify the voices of those with disabilities, so I knew I wanted to continue this work in medical school.
Fortunately, a group of University of Michigan medical students also recognized this and founded the Medical Students for Disability Health and Advocacy (MSDHA) student organization in February 2021 to work to address these issues. MSDHA aims to promote disability health initiatives and support medical students with disabilities and chronic illnesses through education, community building, outreach, and advocacy. The organization strives to create an inclusive community of medical students to support one another throughout medical school and beyond. Creating a community of medical students with disabilities and allies is especially important because only about 1 in 20 medical students report having a disability, which is likely a gross underestimation of the true number of students who identify with having a disability. These students also face unique barriers throughout their medical education.
[Read about the University of Michigan Medical School’s Commitment to Support Students with Disabilities]

Medical students attending a patient panel on the healthcare experiences of Deaf and hard-of-hearing patients.
All medical students are welcome to join MSDHA and contribute to initiatives, plan events, facilitate mentorship, and build community. The organization offers a variety of programs and opportunities, including a near-peer mentorship program called Disability Connect, an American Sign Language (ASL) elective for medical students, hands-on opportunities to work with individuals with disabilities, and public events to spread awareness about disability health topics. In addition, MSDHA hosts social events to strengthen the community.
Recently, MSDHA members hosted a week of educational events designed to supplement the M1 Doctoring course session on Disabilities. The first event was a lunchtime seminar and patient panel consisting of patients and providers describing their first-hand experiences with hearing loss. The next event was a virtual presentation by Dr. Deeba Minhas and Mr. Jared Day surrounding ableism in medicine. We then held a movie screening with a discussion of the award-winning film CODA, a film featuring the perspective of hard-of-hearing individuals, with a catered dinner. Finally, we rounded off this week of events with a seminar given by Anesthesiology faculty on accommodations in the clinical space for students with disabilities.

Attendees at RX to Play Day: Wheelchair Tennis
Another successful series of events that MSDHA has helped organize, along with U-M Adaptive Sports & Fitness and the PM&R Interest Group, is Rx to Play Day. Rx to Play Day is a series of demo days where students have the opportunity to learn how to play various adaptive sports, such as wheelchair basketball and tennis. Jessica Wynne, Head Coach of U-M Wheelchair Basketball, Chuck Aoki, Wheelchair Rugby Paralympian, and Dr. Oluwaferanmi Okanlami, Director of Student Accessibility and Accommodation Services at U-M and Adaptive Sports Director, taught attendees about wheelchair basketball, guided them through drills, and set up a full court game. The goal of the program is to be an informal and safe space to gain experience with adapted sports in the hopes that we can continue to expand awareness and access to health and wellness.

Blake Hardin (M1), Dr. Okanlami, Kate Panzer (M3), and Dana Chung (M1) presenting at the 2023 Diversity in Medicine conference.
As a chapter of Medical Students with Disability and Chronic Illness (MSDCI) National, MSDHA members can collaborate on national disability advocacy initiatives. Medical students have the opportunity to develop advocacy skills, network with like-minded individuals, and work towards creating a more inclusive and accessible medical community across the country.
MSDHA’s initiatives not only benefit medical students but also have a positive impact on the broader community. Through education and advocacy, MSDHA works towards reducing health disparities experienced by individuals with disabilities and chronic illnesses. The organization’s efforts create a more inclusive medical profession that understands and values the unique experiences and perspectives of individuals with disabilities.
MSDHA is an excellent organization for medical students interested in disability health and advocacy. The organization provides opportunities for students to contribute to disability health initiatives, build a supportive community, and collaborate on national advocacy initiatives. MSDHA’s efforts are crucial for creating a more inclusive and accessible medical community that values and supports individuals with disabilities and chronic illnesses at the University of Michigan and beyond.

MSDHA social event at Bitty & Beau’s coffee shop in Ann Arbor.
My involvement in MSDHA has reaffirmed why I wanted to go in medicine in the first place: to advocate and care for patients with disabilities and chronic illnesses by merging compassionate patient-centered care with evidence-based medicine.
by Lisa Chionis | Jul 13, 2023
The polio vaccine. ECMO. The Bovie. These revolutionary medical innovations have not only improved countless lives but also share a common starting point: the University of Michigan Medical School (UMMS)!

Rising M4 students celebrate the completion of their I&E Capstone projects
As UMMS students, we are fortunate to walk the same halls where brilliant minds have dedicated their efforts. Now, it is our turn to contribute to the strong tradition of innovation and entrepreneurship (I&E) at Michigan.
A recent symposium united medical students who are dedicated to advancing healthcare through innovation, whether it’s leveraging technology, conducting research, or reimagining healthcare systems.
The day began with design thinking presentations by three teams of M1 students. These teams had collaborated on projects for months, utilizing the five phases of design thinking to tackle patient challenges. By empathizing, defining, ideating, prototyping, and testing, they devised innovative solutions aimed to improve the patient experience and health outcomes.
One standout project by “Team Zopf” addressed the concerns of a parent caring for a young patient with amyoplasia. The parent frequently monitored their child’s O2 saturations and performed jaw thrust maneuvers to relieve airway obstruction. Their solution? A low-cost, adjustable device that mechanically maintained the jaw in an elevated position while employing continuous O2 monitoring to alert the parent of prolonged desaturation events.
This solution not only showcased Team Zopf’s empathy towards the parent’s desire to avoid additional surgeries but also demonstrated their creativity – utilizing household objects to craft a functional prototype – and their scientific expertise – explaining an impressive torque diagram and 3D CAD model. They discussed next steps for their design, including prototyping and testing, navigating the regulatory pathway, large scale manufacturing, and determining the market value and impact.

Team Zopf’s Design Thinking presentation (Members: Mike Allevato, Dhanya Asokumar, Mikoto Kobayashi, Anna Riegger, James Schlabach, Jasnoor Singh, Sunny Singh, Daniel Wieczorek, Hannah Xu, and Jess Yen)
The symposium also provided the opportunity to learn from influential voices within our University of Michigan innovation community. We heard from our I&E Path Co-Directors, Dr. David Zopf (Pediatric Otolaryngology-Head & Neck Surgery) and Dr. Sonal Owens (Pediatric Cardiology), and Michigan Medicine surgical residents Dr. Jaes Jones (Neurosurgery PGY-4) and Dr. Taylor Kantor (Integrated Cardiothoracic Surgery PGY-5). The panel explored applications of 3D printing in surgery, virtual reality (VR) in medical education and patient care, and the relationship between industry and academia.
A highlight of the panel was Dr. Owens sharing her experience collaborating with the Stanford Virtual Heart experience, which has now evolved into the Michigan Anatomic Congenital Heart in 3D (MACH3). As M2 students on the Pediatrics rotation, my classmates and I had the opportunity to immerse ourselves in a virtual heart, exploring chambers, vessels, and learning cardiac anatomy. The integration of VR into our curriculum added a whole new dimension to our learning, and I eagerly await its further incorporation. Dr. Owens’ announcement that the new MACH3 program will lead the development of a hypoplastic left heart syndrome (HLHS) module filled the room with excitement. It’s incredible to witness the advancements happening at UMMS in real-time!

Medical students were all ears for Drs. Jones, Kantor, Owens, and Zopf
Next, we moved into M4 presentations. Demetri Monovoukas and Nick Zugris shared their journey launching Scalpel – a free online platform that offers foundational surgical training (think Khan Academy for the Surgery rotation), while also providing 3D printed hardware for suturing practice. Kian Pourak unveiled a 3D-printed surgical knot tying device designed to help trainees master the art of tying knots at the optimal tension, and Michelle Benedict shared a video documenting her experiences working at Apple before entering medical school, adding another unique perspective to the mix.
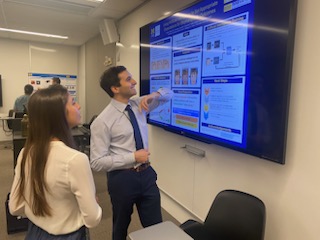
The symposium’s grand finale was a poster session in Taubman Health Sciences Library, inviting students from all classes to explore the capstone projects of rising M4 students. These capstone projects, a requirement for graduation from the I&E Path of Excellence, showcased students’ innovative laboratory endeavors, collaborations with startups, quality improvement projects, and more. The poster session fostered connections between M1s and rising M4s, who were on the lookout for successors to carry forward their projects once they graduate.
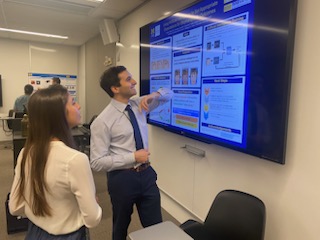
Jeremy Shapiro (rising M4) presents his research using AI to predict blepharoplasty outcomes
As UMMS students, we have the incredible challenge, privilege, and responsibility to carry forward the legacy of medical innovation. We invite incoming students to join us on this mission through the I&E Path of Excellence. Mark your calendars for the 2nd Annual I&E Symposium in June 2024 – all students welcome!
by Jasnoor Singh | Jul 6, 2023
Michael was an eclectic 13-year-old boy that I met during my time as an undergraduate in Biomedical Engineering at Michigan. He was often the loudest, proudest voice in the room and always primed with sporadic conversation topics. As a below-elbow amputee, he had just three design requirements for the 3D-printed prosthetic arm that a team of students and I spent a year creating for him. “Make sure I can tie my shoes with it, make it look like the Terminator’s bionic arm, and make sure I can do multiple pull-ups.” Could a plastic, multicolored, actuated arm design by engineering students accomplish this? To Michael, his disability was really an opportunity to create an assistive medical device that others would marvel at.

An example of a low-cost 3D-printed prosthetic hand made by students at the University of Michigan.
This was my first-ever customer discovery interview. It launched me into a focus on 3D-design, additive manufacturing, and biomechanics during my education. With abundant open-ended design problems in healthcare and engineering, my experience at Michigan taught me to meticulously explore design features, learn to develop the skills needed for a project, and leverage the bright minds and endless resources around me to avoid settling on the answer, “it can’t be done.” I related to Michael in that, when I was a young boy, I never wanted to hear no as an answer. Today, I try to approach innovation, frustrations, and even daily life setbacks with a “challenge accepted” mindset. I hope to serve my patients and colleagues to my full potential with this in the future.
After I started my first year of medical school at the University of Michigan, my first thought was, “well, there goes my engineering degree!” We don’t always cover complex fluid models of the body’s vasculature or learn about in-depth mechanics of interactions between bones/joints (I’m sure my classmates are grateful). We learn practical ways to diagnose, treat, and understand why diseases behave the way they do. But beyond coursework, I have found many ways to keep my spirit of innovation fueled at Michigan. The first was Sling Health, where we formed a project team led by my fellow M1, Danika.
Danika shares my spontaneity in thought, my level of detail in drafting emails, and my desire to painstakingly and completely explore ideas. She brought us together around the goal of addressing a pressing need in healthcare: development of a non-invasive anticoagulant solution that improves extracorporeal membrane oxygenation outcomes and lower costs. ECMO is a technology that acts as an artificial heart or lung for critical care patients who cannot provide enough blood flow or oxygenation on their own. Preventing blood clotting complications within ECMO circuits has great potential to prevent strokes, pulmonary emboli, and numerous other costs and downstream effects.
Our team members also include engineering and business students: Liam, Nundini, Carol, and Noor, who all have experiences ranging from venture capital, research in coagulation and thrombosis, robotics, and even ECMO itself. I absolutely admire Danika’s dedication to involve all members of our team and regularly find resources to support members who are new to ECMO and engineering design. As future physicians, the need to explain complex topics in streamlined ways is so important, and being part of a multidisciplinary team necessitates this. Soon enough, we branded ourselves “EmboFlux.”
Almost immediately, we ran into limitations. It would be much easier to create a device that detects clots rather than dissipates them. Biocompatible device regulatory cycles are also incredibly lengthy and costly if our device was required to interface with blood in any way. Numerous customer discovery interviews pointed this out to us. Time and resources are a major barrier for startups or device design groups. But by exploring prior patent art and recent developments in anticoagulation therapies, our team found a novel way for reducing anticoagulation without directly contacting blood, which allows us to shorten the regulatory timeline and save costs. This was an idea that many clinicians and ECMO researchers were supportive of.
Our team initially competed in the campus-wide Michigan Business Challenge. We’ve received great support and mentorship from Anne Perigo at the Zell Lurie Institute, who worked with us to refine and pitch the importance of our design problem to judges and investors. Anne never hesitated to meet with our team weekly or recommend further individuals to contact for support. What I admire about Emboflux is that our members leveraged almost every resource available to conduct research before launching into device design. We thoroughly defined our problem, referenced existing literature, devised market estimates, and explored competitive solutions. EmboFlux was fortunate to make it to the semi-finals of the Michigan Business Challenge, and we look forward to competing again in future years!
I remember a conversation I had with Danika within our first few months. We marveled at how open and supportive the Michigan Medicine community was to us when we were seeking advice on device design, clinical adaptation, and even devising our first few research studies for the EmboFlux prototype. With a mix of initial intimidation but also intrigue, I truly believe medical school is a great time for innovation. In our flexible M1 curriculum, Danika and I can schedule device tests or attend pitch competitions during the week and complete our curricular requirements and assessments around our schedule, even into the weekend. This has made it easier for us to balance the many duties of a design team with the responsibilities of medical students. The Extracorporeal Life Support Lab at the University of Michigan has also been incredibly supportive in allowing us to conduct tests and receive feedback on device design.
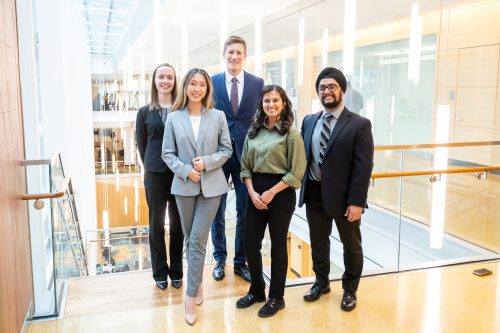
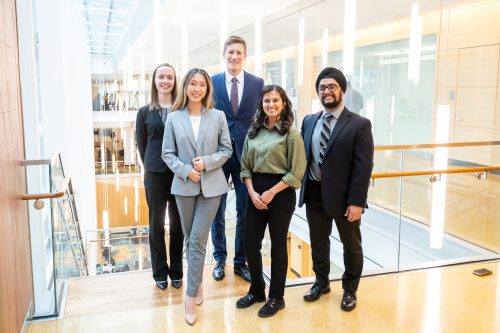
From left to right, Danika Meldrum, Carol Dai, Liam Mathews, Nundini Rawal, and Jasnoor Singh. This is a photo of our team after competing in the Michigan Business Challenge held at the Ross School of Business.
While many of us are new to surgical settings and adapting medical devices effectively, our team also took part in the Surgical Innovation Discovery Course through the Center for Surgical Innovation. Here, we received guidance in prototyping Emboflux for clinical adaptation and conducted more customer discovery interviews to showcase our design and aim for perpetual refinement. With device design comes continuous iterations and regular communication with experts to add modifications or features. Customer discovery will remain a vital part of our team moving forward, and it’s also incredible that we can think of many more stakeholders and bright minds at Michigan we have yet to meet, and that they would have such insightful input for our EmboFlux device. With feedback and advice from Candice Stegink, Jon Campbell, and the many surgical solution experts through SIDC, we really developed a clearer picture of how EmboFlux could find its way to ICUs and ECMO patients without disrupting existing workflows. The healthcare setting provides a whole new set of design criteria I’ve never really experienced in past projects. It has thus been super valuable to have resources like residents, surgical mentors, and researchers so close for advice.
In April 2023, our team was invited to present and pitch EmboFlux at the National Sling Health Demo Day in St. Louis. It was here that we presented our work exploring our clinical problem, market, and initial benchtop studies in a five-minute on-stage pitch. While we were anxious about our presentation or about the questions judges might counter with, we were excited to interact with many individuals who were incredibly curious about EmboFlux. Ranging from surgeons literally on call during the event to undergraduate students, we walked away with numerous contacts for future potential collaborations. We also witnessed presentations from up-and-coming medical devices all designed by future engineers, doctors, and innovators. After an incredible pitch from our spokespersons, Liam and Danika, we were so grateful to have received the National Demo Day’s 1st place award and audience choice for best pitch!
 Within our team, I’ve especially admired how individual members are so confident and willing to take initiative on different aspects of our design work. We all bring technical design skills, but our background in ECMO technology, hemostasis research, and effectively pitching to investors has been valuable in creating a well-rounded, multidisciplinary team that can respond to each new problem with “challenge accepted.” I have self-reflected and can think about multiple times where I was unsure of specific aspects of medical device development, regulatory guidelines, the business side of medicine. But so often, I am met with unwavering resolve from our other team members to find the resources necessary to make our path forward more clear. This helps me reinforce my belief in my own abilities and encourages me to approach ambiguity with confidence and intrigue.
Within our team, I’ve especially admired how individual members are so confident and willing to take initiative on different aspects of our design work. We all bring technical design skills, but our background in ECMO technology, hemostasis research, and effectively pitching to investors has been valuable in creating a well-rounded, multidisciplinary team that can respond to each new problem with “challenge accepted.” I have self-reflected and can think about multiple times where I was unsure of specific aspects of medical device development, regulatory guidelines, the business side of medicine. But so often, I am met with unwavering resolve from our other team members to find the resources necessary to make our path forward more clear. This helps me reinforce my belief in my own abilities and encourages me to approach ambiguity with confidence and intrigue.
Beyond these experiences, numerous other spaces and opportunities within our medical school will allow me to continue exploring my interests in engineering and design through the Innovation and Entrepreneurship Path of Excellence, I have already gained vital exposure to design thinking principles and effective interview strategies. Recently, we received the opportunity to interact with patients and brainstorm a user-specific design solution in an ongoing process. I was able to see my colleagues shine and show their willingness to fully explore a healthcare concern prior to proposing innovative ideas. My fellow classmates truly are so multi-faceted, and the field of innovation and design is so fulfilling, even for anyone who may not have a technical background. Your curiosity and novel ideas are always welcome!
In the future, I hope to work on medical device design in low-resource areas, where user-friendly, low-cost, and quickly adaptable engineering devices can be beneficial to address healthcare concerns for underrepresented patients. I look forward to clinical rotations in the coming year, where I will develop even more exposure to workflow and areas of innovation possible in a healthcare setting. Our EmboFlux team also looks forward to further pitch competitions, solution refinement workshops, and helping prevent many complications of ECMO procedures!
by Matt & Patty Friedland | Jun 15, 2023
Hi, everyone! It’s been a while since we’ve written for Dose of Reality. A lot has happened since our last post in 2020… We hope everyone is caring for themselves and their loved ones as we transition out of the acute COVID era.
 For us, we have a couple of updates to share:
For us, we have a couple of updates to share:
1. We got married in August 2022 in a small wedding in New York’s Hudson Valley with close family and friends.
2. We are now proud dog parents to a 3-year-old puppy named Georgie.
3. Patty now works for Duo Security here in Ann Arbor as a Customer Solutions Engineer, while Matt recently finished his MBA year at the Ross School of Business. He is preparing to re-enter the medical school world later this summer and apply to residency programs this fall.
The Challenges of Giving Advice
Giving advice is difficult as every person has their own unique experience, so we tried to be thoughtful about choosing 10 universally applicable ideas that might resonate with others on the same journey. Reflecting on our medical school experience was a helpful exercise. In preparing for this post, we discussed our highs and lows to distill what worked best for us and what we might have done differently.
Some highs of medical school included finishing the USMLE exams, finding my passion in medicine, meaningful patient encounters, connecting with mentors and celebrating our life outside of school – weddings, travel, birthdays and dog birthdays. Some lows of school are the ones you can imagine; it’s a challenging four years filled with frustration, stress and many missed events. We hope these 10 pieces of advice can be a jumping-off point for reflection and conversation between you and your partner.
Please know that what worked for us may not work for you, but discussing these principles may help shape your experience. The ultimate goal is to be intentional about the life you are building together.
Lastly, before we get to the advice, a framing that has been helpful for us is to intentionally choose to see life as an adventure. Adventures have both rewarding and challenging parts, but everything is part of the plot. This lens has been a beneficial filter when times are tough because highs and lows are both part of the expected path on any adventure. Now, onto the advice!
 10 Tips for Navigating Med School with a Partner:
10 Tips for Navigating Med School with a Partner:
1. Open communication: This sounds cliché, but it’s truly the key to any successful partnership. Both people should equally share their feelings, concerns and expectations with one another. These may change over time, and disagreements will arise, but it’s important to know how each other is doing, how they feel and how you can be supportive. Medical school, personal life, job, etc., all come with difficulties, so set aside time a few days per week to give honest updates about your life, work, finances, health, struggles and triumphs.
2. Understand the demands: This is one of the more challenging aspects of medical school. Students generally don’t know exactly what is expected of them or how they’ll need to allocate time, but do your best to understand and communicate what is expected of you. It can be hard to explain the exact situation and expectations of medical school but proactively share that information, as it helps to set reasonable expectations. As they say, disappointment is the difference between expectation and reality.
3. Create a realistic schedule and prioritize time together: Your calendar is your friend. Be sure to add all of your obligations, study time, exercise, gatherings with friends and partner time on there. This helps you be intentional about how you spend your time and serves as an exercise in setting priorities. Set a recurring block in your calendar that is protected time to spend with your partner. This can be for catching up, having dinner in town or doing your favorite activity together. Show me your calendar, and I’ll show you your priorities.
4. Be flexible and understanding: Medical school is often unpredictable, and some months are busier than others. Plans may need to be changed or canceled at the last minute. It’s frustrating, but it happens. Both partners should be adaptable and flexible when this occurs. Do your best to set aside protected time and communicate the need for flexibility.
5. Take care of yourself: Both partners should prioritize self-care and maintain their own physical and mental well-being. This may cut into some personal time, but it’s important to encourage each other to pursue hobbies, exercise and maintain a healthy lifestyle. Having independent lives and interests helps when schedules are hectic and you find yourself without something fun to do. View taking care of yourself individually as a way to support each other as a couple.
6. Celebrate milestones and achievements: Medical school is a long journey, and it’s important to celebrate milestones and triumphs along the way. Whether it’s finishing an exam or a hard rotation, take the time to acknowledge and celebrate these accomplishments together. This can be anything from a handwritten card to a nice dinner. Time passes quickly, so be sure to find reasons to celebrate together.
7. Seek support from others: Both partners should reach out to friends, family or groups in the community for additional help when needed. Having a network of people who understand the challenges of medical school is a valuable source of support and encouragement. The Medical School Mental Health Program now has robust resources for students to use, so reach out and see how they can help!
8. Practice patience and resilience: Medical school can be stressful and exhausting, but it’s temporary. It’s not always easy, but view this as an opportunity to prove to yourself the ability to overcome challenges. You are both working towards a common goal; relationships often grow stronger through shared challenges.
 9. Assume good intentions: It is a long road, and some days it is hard to maintain a positive outlook. When someone makes a mistake or things do not go according to plan, it is best to default to assuming good intentions. (This is a powerful default in life, too – see ‘This is Water’ by David Foster Wallace). And, as Ted Lasso says, ‘Be curious, not judgmental.’
9. Assume good intentions: It is a long road, and some days it is hard to maintain a positive outlook. When someone makes a mistake or things do not go according to plan, it is best to default to assuming good intentions. (This is a powerful default in life, too – see ‘This is Water’ by David Foster Wallace). And, as Ted Lasso says, ‘Be curious, not judgmental.’
10. ‘Things are rarely as good or bad as they seem’: This is a motto we deeply resonate with. The bad isn’t always as bad as it initially seems, and the same with the good. Life is complicated and full of tradeoffs, so it is crucial to keep moving forward with equanimity, optimism and curiosity. What may seem difficult in the short term may be a blessing over time. Ok, this is the last cheesy quote of the article, I promise, ‘there is nothing either good or bad, but thinking makes it so’ from Hamlet.
Every relationship is unique, and it’s essential to find what works best for you as a couple. Hopefully, these are some universal considerations to discuss and agree upon while going through school and training. We encourage you to revisit these topics with each major change in schedule as the demands of school and home fluctuate. It is definitely possible to maintain a happy and healthy relationship while in medical school, but it requires open communication, prioritizing quality time, patience, support, empathy and compromise. Be intentional and enjoy the adventure!
Wishing you the best, Matt & Patty Friedland
by Ellery Sarosi | Jun 1, 2023
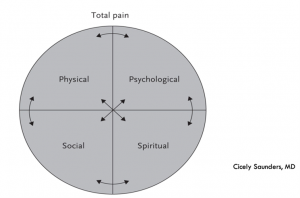
Out of the countless PowerPoint slides from M1 year, there’s one that, four years later, I can still picture with absolute clarity. Presented in coordination with the University of Michigan Medical School’s Program on Health, Spirituality and Religion (HSR), the slide was part of a lecture on attending to the religious and/or spiritual identities of our patients, and it portrayed the Theory of Total Pain. Proposed by the founder of modern hospice, Dr. Cicely Saunders MD, this theory describes suffering as the sum of a patient’s physical, psychological, social, and spiritual distress. This slide and its message has stuck with me as, over the course of medical school, I have seen Dr. Saunders’ multidimensional view of health and suffering come to life in the stories of my patients.
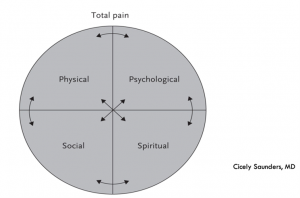
Figure 1: Dr. Cicely Saunders’ Theory of Total Pain
As clinical students, we have the privilege of accompanying people during some of their most joyous and some of their most challenging moments. These patient relationships range from witnessing someone deliver their newborn baby to walking alongside someone mourning the reality that they are dying. While at vastly different ends of the emotional continuum, a common thread connects these two relationships. Both prompt a sense of wonder about how patients and their loved ones navigate such significant moments of transition. It’s in these moments where it becomes particularly clear to me that the practice of good medicine demands both provision of excellent biomedical care as well as a willingness to connect, person to person, with the human sitting in front of me.

Our HSR Welcome Dinner, a time for medical students and HSR core faculty members to connect, reflect, and eat good food!
Within this connection, patients consistently teach me about Dr. Saunders’ theory of medicine in conveying that health is not solely biological or physical, but together with other essential dimensions of health and personhood – health is also psychological, emotional, social, and spiritual. Their instruction to me of these dimensions comes in many forms: a request to keep family informed about clinical updates, an inquiry about Halal food options in the cafeteria, a desire to spend time outside in the midst of a long hospital admission. It is these lessons about the multidimensional nature of health and suffering that have led me to dive into all that the HSR Program has to offer.
The HSR Program was created in 2017 with the mission of developing opportunities for medical trainees and physicians to explore the intersections between health, spirituality, and religion. Broadly speaking, spirituality is anchored in where an individual finds meaning, whether that be in a world religion, nature, family, music, etc. Our exploration of this intersection occurs through lectures, research, and interdisciplinary training and is all geared towards enhancing patient centered care and encouraging personal meaning making in the practice of medicine. With this mission in mind, we host a speaker series, create courses/curricula on health, spirituality and religion and mentor students on how their religious and/or spiritual identity contributes to their professional identity formation. This innovative program is led by an incredibly kind and thoughtful group of attending physicians, Drs. Kristin Collier (Internal Medicine), Jeremy Baruch (Psychiatry), Adam Baruch (Ob/Gyn), and Phil Choi (Pulmonary & Critical Care).
To expand further upon opportunities for engagement with the HSR Program, I want to share some of my highlights from my involvement. Our monthly Woll Family Speaker Series on Health, Spirituality and Religion (an opportunity that is open to all who are interested!) brings in speakers who share how the intersections between HSR are apparent in their own experiences with patients. We’ve heard lectures from physicians affiliated with the University of Michigan, including our own Dr. Scott Stonington, an Internal Medicine physician and anthropologist, who presented a talk entitled “Working the Mind-Body: Discomfort and the Pragmatics of Spirituality (in Thailand and the U.S.).” We also bring in speakers from other institutions. Recently, we hosted Dr. Rita Charon, an Internal Medicine physician at Columbia University and literary scholar credited with creating the field of Narrative Medicine, who led an interactive discussion entitled, “Native Fusion: Creativity, Responsibility, Meaning,”. These seminars have led to rich discussions about the nature of suffering and what it means to be healthy, all the while building up a sense of community among students, faculty, staff, and members of the Ann Arbor area who are interested in engaging with such questions of humanity and healthcare in all its fullness.
In addition to the seminar series, all medical students rotating through an intensive care unit (ICU) have the opportunity to participate in the HSR Program’s Healing Presence elective, which I participated in during my Pediatric ICU rotation. The ICU directors love Healing Presence and encourage all medical students to partake. For participating students, you have the opportunity to develop new patient care skills focused on the spiritual needs of your patients. This development occurs through rounding with chaplains in the ICU during which you have the chance to explore various skills such as taking a spiritual history, providing supportive listening, and sharing healing words/prayer. You also engage in a structured, small group facilitated by a chaplain to process your own experience working with critically ill patients and their families. Personally, the Healing Presence elective helped promote my wellbeing while on an intense rotation and has helped me feel more equipped to attend to the spiritual distress of my patients and to work effectively with Spiritual Care colleagues.

Presenting the Conference on Medicine and Religion workshop that Dr. Baruch and I created.
At the core of my experience with the HSR program has been the longitudinal mentorship I received. What started with a “cold email” sent near the beginning of M1 year has turned into what I hope will be lifelong mentoring relationships with Drs. Kristin Collier and Adam Baruch. Through their mentorship, I have grown personally and professionally and added depth of meaning to my understanding of the practice of medicine. They have opened the door to unique opportunities for scholarship. I’ve contributed to curriculum development, specifically working alongside attending physicians and other medical students to evolve in the Doctoring session on “Religion and Spirituality in Patient-Centered Care.” In coordination with Dr. Collier, I’ve co-presented a talk entitled, “Whole Person Care” at a Continuing Medical Education event hosted by Michigan Medicine. I’ve collaborated with Dr. Baruch in conducting an Ob/Gyn Grand Rounds presentation and a Conference on Medicine and Religion workshop, both of which were entitled, “Cultural and Religious Humility: A Foundation for Relationships in Medicine.” With the help of another medical student, we’ve subsequently turned these presentations into a manuscript that is pending submission.
These mentoring relationships and my engagement with the HSR Program has culminated in being the inaugural student fellow for the program during the 2022-23 academic year. Within this role, I’ve had the privilege of helping develop our programming through participating in regular HSR core faculty meetings, helping select speakers for the Woll Family speaker series, providing near-peer mentoring of a clinical trunk student, and cultivating a community among students interested in what the HSR Program has to offer. Having wrapped up medical school, I’m thrilled to know that three, all-star medical students will step into the role of HSR student fellow for this upcoming academic year. I can’t wait to see how they help shape the HSR Program and community!
While I’m immensely proud of our scholarly work, what is most significant to me is the way I anticipate this work finding expression in my practice of medicine. As I look ahead to July and the start of my OBGYN residency at the University of Michigan (Go Blue!), I’m confident that my involvement in the HSR Program will continue to come to life in the patients I help care for and in the ways they will take up Dr. Saunders’ torch in teaching me about health and suffering as the sum of their physical, psychological, social, and spiritual states. And more personally, I’m grateful for the ways that my role as an interested student, mentee and fellow continue to help me feel more deeply connected to sources of meaning in medicine, a gift that feels particularly significant amidst the crisis of physician burnout.

A fun dinner outing with core faculty for the HSR Program!
The HSR Program has so much to offer the intrigued Michigan medical student. Opportunities abound both for dabbling in our programming and for more in-depth exploration. You can find these opportunities summarized on our website, and while you should absolutely explore this webpage, I would be remiss if I didn’t encourage you to reach out to talk with us! At the core of this Program’s mission is its commitment to personal connection with students who have never had the opportunity to explore this space or who wish to dive deeper into this space of whole person care. If you find yourself interested, please reach out! You can connect with me at sarosie@med.umich.edu or message our HSR Program email at Health.Spirituality.and.Religion.Info@umich.edu. Whether you’re a current or prospective medical student, we would love to hear from you!
 It is an honor to be with patients in these moments and support them in ways that we can. However, sometimes it feels like there are constraints within the healthcare system — we leave these patient interactions wishing there was more we could do to change these peoples’ circumstances. This desire to drive positive change for patients beyond the one-on-one clinical setting often takes shape in the form of advocacy work.
It is an honor to be with patients in these moments and support them in ways that we can. However, sometimes it feels like there are constraints within the healthcare system — we leave these patient interactions wishing there was more we could do to change these peoples’ circumstances. This desire to drive positive change for patients beyond the one-on-one clinical setting often takes shape in the form of advocacy work.  At the end of the course, students had the opportunity to travel to Lansing, where they spoke with Washtenaw County’s Rep. Carrie Rheingans and Sen. Jeff Irwin. Some students interested in emergency medicine elected to travel to Washington, D.C. and attend the American College of Emergency Physician’s Leadership and Advocacy Course with Dr. Uren. In future classes, students may also travel to the American Medical Association’s National Advocacy Conference in Washington DC. Other opportunities may be available for students with other specialty interests as well.
At the end of the course, students had the opportunity to travel to Lansing, where they spoke with Washtenaw County’s Rep. Carrie Rheingans and Sen. Jeff Irwin. Some students interested in emergency medicine elected to travel to Washington, D.C. and attend the American College of Emergency Physician’s Leadership and Advocacy Course with Dr. Uren. In future classes, students may also travel to the American Medical Association’s National Advocacy Conference in Washington DC. Other opportunities may be available for students with other specialty interests as well.









 Within our team, I’ve especially admired how individual members are so confident and willing to take initiative on different aspects of our design work. We all bring technical design skills, but our background in ECMO technology, hemostasis research, and effectively pitching to investors has been valuable in creating a well-rounded, multidisciplinary team that can respond to each new problem with “challenge accepted.” I have self-reflected and can think about multiple times where I was unsure of specific aspects of medical device development, regulatory guidelines, the business side of medicine. But so often, I am met with unwavering resolve from our other team members to find the resources necessary to make our path forward more clear. This helps me reinforce my belief in my own abilities and encourages me to approach ambiguity with confidence and intrigue.
Within our team, I’ve especially admired how individual members are so confident and willing to take initiative on different aspects of our design work. We all bring technical design skills, but our background in ECMO technology, hemostasis research, and effectively pitching to investors has been valuable in creating a well-rounded, multidisciplinary team that can respond to each new problem with “challenge accepted.” I have self-reflected and can think about multiple times where I was unsure of specific aspects of medical device development, regulatory guidelines, the business side of medicine. But so often, I am met with unwavering resolve from our other team members to find the resources necessary to make our path forward more clear. This helps me reinforce my belief in my own abilities and encourages me to approach ambiguity with confidence and intrigue. For us, we have a couple of updates to share:
For us, we have a couple of updates to share: 10 Tips for Navigating Med School with a Partner:
10 Tips for Navigating Med School with a Partner: 9. Assume good intentions: It is a long road, and some days it is hard to maintain a positive outlook. When someone makes a mistake or things do not go according to plan, it is best to default to assuming good intentions. (This is a powerful default in life, too – see ‘This is Water’ by David Foster Wallace). And, as Ted Lasso says, ‘Be curious, not judgmental.’
9. Assume good intentions: It is a long road, and some days it is hard to maintain a positive outlook. When someone makes a mistake or things do not go according to plan, it is best to default to assuming good intentions. (This is a powerful default in life, too – see ‘This is Water’ by David Foster Wallace). And, as Ted Lasso says, ‘Be curious, not judgmental.’